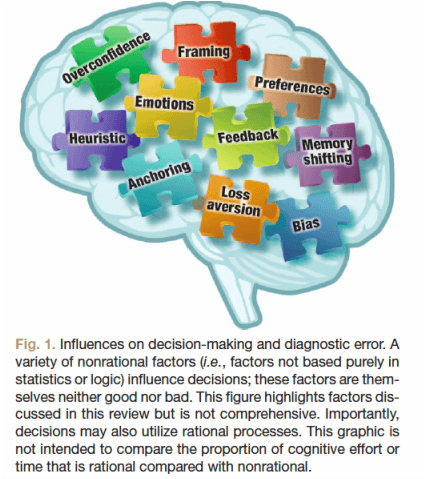
What are the processes that contribute to errors in medical decision making? Certainly, medical decision making is complex, and simple knowledge gaps could be to blame. But very often, experienced physicians make medical decision errors in the form of cognitive errors. Cognitive errors are thought process mistakes frequently rooted in nonrational decision processes, rather than knowledge gaps. What is a nonrational cognitive process? Simply put, this term refers to proceses that are not rooted strictly in statistics. Nonrational is not intended to be synonymous with ridiculous or unreasonable, just not purely mathematical. The figure below, from Anesthesiology, shows a few examples of nonrational influences on medical decision making (and all other kinds of human decision making!).
Although we often think of ourselves as logical and rational (we’re scientists, after all), purely logical methods may not be ideal for medical decision making for a few key reasons:
1 – We do not have complete certainty about all the possible choices. Unlike a coin toss, in which there are two known possible outcomes, constellations of signs and symptoms are much less definitive.
2 – We do not have complete certainty about the probability of each choice in our patient. True, some population based data does help us decide “pre-test” and “post-test” probabilities overall, but these numbers do not always apply to the patient in front of us.
3 – We do not have complete agreement on the preference order for each outcome of our decisions. Preferences vary from patient to patient, and from physician to physician. So, even if we had complete certainty in items 1 and 2, “rational” decision making still fails us when it comes to personal preference.
“Abundant evidence suggests that real-world
medical decision-making is beset with variability and complexity.
Physicians often fail to agree on the interpretation of
diagnostic test result, are inconsistent in their approach
to management, and arrive at different diagnoses in the
presence of identical information. Even for clinical conditions
with a widely accepted theoretical framework, a startling
amount of unexplained practice variability exists.”
Consider, for example, a patient who has suffered a brain injury and is in a coma. In some cases, prognosis seems clear. However, there are many cases in which one cannot say with certainty whether recovery is possible, and if so, how long might it take, at what expense (psychologically and perhaps monetarily), and what level of function or quality of life can be achieved? Even if these questions could be answered with complete certainty, patients and their families are likely to have a wide variety of opinions on what decision processes and outcomes would be acceptable. Or, consider the patient who has a religious objection to receiving a blood transfusion, and would rather die than receive one. This situation illustrates a patient preference, and the caregivers who would have to withhold lifesaving treatment in dire circumstances may also have preferences about their own decision behaviors.
These nonrational preferences are important, and guide our medical decision making in a way that is not easily represented via statistics or accounted for in a Bayesian model. What implications does this have for our current paradigms of “evidence based medicine” and “patient centered care”?